Contributor: Dr. Suman Chowdhury, Ex- Medical Officer, Chitagong Medical College Hospital
Approach to Unconsciousness
—————————————————
Well, though no GP will have (except very rare occasion) to face an Unconscious patient, yet it is of great concern not only for Dx and Mx but also for the attending relatives!
Here, Unconsciousoness will signify the state of Coma. And Coma is defined when GCS (Glasgow Coma Scale) score is less than 8.
I’m not going to the details of GCS and pathophysiology of coma here, as all of you must have known this.
In every emergency and Accident department of any hospital has to receive thsese kind of patients.
The anxious and agitated attendants rush there with the hope of recovery from Unconsciousness. They want it immediately and sometimes take it so seriously that even their behaviour may influence the surrounding environment of the Mx. Because, unconsciousness is second to death to most of them!
But, most important thing is to act just reverse (don’t need to show that) to the attendants as a physician! That means, to be calm enough and steady, to drive into the sea of thought to find out the etiology.
Because, the exaggeration and aggressive attitude (in management) of the attending physician will not make the Unconscious patient (truly) be conscious one, unless the unconsciousness is due to hypoglycaemia!
So, In any case seems to be organic one, Always go for CBG (Capillary Blood Glucose). Its mandatory!
If (and only if) it is normal, then go for finding the etiology. Because, (Remember) hypoglycaemic patient may be admitted with bizarre presentation which greatly mimics various features of stroke, Metabolic encephalopathy, ICSOL and what not!
(Although, the classical features should have been known to all)
Now, to limit the opening of the window of Thought, the Following points are to be noticed:
1. Extreme of ages (too young to too old) almost always have organic etiology
2. Female of late teen to early thirties almost have non organic causes
3. Unknown male patient almost always have history of Transport (commuter) poisoning
4. known middle aged male have various pathology
5. Middle aged women are less found (may be they have to serve the rest of the group)!
Unconscious patient cannot provide any history. But a truly Unconscious (i.e, not of simulated coma) can’t hide most of their physical findings, and we have to reveal them during physical examination!
Inspite of that, try as much as u can to collect the history as much as you can.
Selection of person to have a proper history is very much important. Because, wrong or half truth history may misguide us and take away valuable time.
Who can be good candidates:
————————————————
1. Patient’s mother or father
2. if not available, patient’s brother and sister
3. If not available, patient’s closed friend
4. If not available, patient’s neighbours who take him to the Hospital or physician
If none is available, then its YOU and Your CLINICAL JUDGEMENT which will ultimately help reach a provisional Diagnosis.
Which points to be touched During taking history:
—————————————————————————
1. Onset: Gradual or sudden
2. Preseced by fever or not
3. Any co morbidities (DM, HTN, CKD, COPD, Hepatic illness etc)
4. Any history of Epilepsy
5. Any history of Drugs like Thiazides etc
6. Any history of travelling to Hill Tracts
7. Any significant history of mental depression or Psychiatric illness
8. Any history of Drug abuse or addiction etc.
Presence of fever narrow down the DDs.
– If fever preceded:
Unconsciousness, Infective causes are likely (Cerebral malaria, encephalitis, meningo-encephalitis, sepsis due to any cause ).
– If fever comes later:
ICH (Specially Pontine) and Metabolic causes are to be considered.
Some interesting points:
—————————————-
1. In extremely old patients, the following causes are more likely:
* Dyseletrolytaemia (Hyponatraemia)
* Hypoglycaemia
* Respiratory and Urinary infection
* Respiratory failure from COPD
* Acute or Chronic subdural haematoma
* Victim of transport poisoning etc.
2. Young male:
* Massive ICH (Intracranial haemorrhage)
* Brain stem stroke
* Transport poisoning
* Narcotic drugs taking (with intention to self harm)
* Any metabolic causes due to previous chronic illness
3. Young female:
* Pseudo unconsciousness due to a part of Conversion disorders
Narcotic drugs overuse as a way to self harm
* Viral encephalitis etc.
Though anything can happen to any patient!
Now, During examination, we have to get maximum information to formulate the etiology of unconsciousness.
Examination of any unconscious patient needs attention to some special region rather than examining them as a whole (usually done in any conventional ill person). It can be termed as CUSTOMIZED examination.
The regions are:
—————————
* Examination of Eye
* Examination of CNS function by eliciting long tract sign (upper motor neuron sign), such as extensor planter response etc.
* Ovserving the breathing pattern
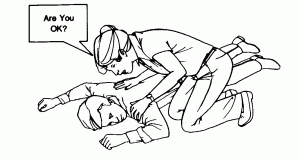
When there is no significant history to guide towards some specific etiology, start examining the patient by calling by name. If necessary, a bit loudly near to his ears.
If non responsive, keep pressure (over the sternum by knuckles along with shouting.
Meanwhile, look at the eyes, change in posture or any slight movement of any parts of the body (uppr or lower l8mbs, corner of moth, opening of oral orifice or eye movement.
Factors indicating conversion disorders or Simulated Coma (where the patient tries his best to be in coma!):
1. Rapid movement of eyeball with closed lids
2. Forceful closure of eye on passive opening (by doctors)
3. The eyes point upwards exposing the conjunctiva (Bell’s sign), suggesting his intention to close the lids.
4. After opening (by the physician) the patient try to close the lids again rapidly.
Posture of the Patient:
————————————
1. Usually lie in supine
2. Try to remain as straight as he can
3. Usually all major joints remain in exceptionally extensor position.
Pupil:
——–
Will remain normal characterised by:
– Normal and equal size of both pupils
– Normal reaction to light (Light reflex).
Additional tests:
1. Lifting one of the upper limbs, holding it in raised position for a while and suddenly allowing it to fall just over his (patient’s) face
Any of the followings or all are suggesive of Simulated Coma:
* A sustained posture of that limb in raised position
* Technically (cleverly) avoiding his face while the limb was allowed to fall free
* Sudden cease of that limb while the was let to fall down
2. Closing both nostrils tightly (ensure that no air leaks) with the hands of the physician suddenly
Patient can’t tolerate it for long and as a consequence he is compelled to open hhis mouth to breathe.
Suspicious history and Positive results of the abovementioned examination almost invariably indicate the Simulated coma or Conversion (functional) disorder.
Suspicious history:
——————————
* History of familial dispute (among parents, husband-wife, brother-sister, beloved one etc)
* Finding empty strips of sedative in the room
* Positive history of drug abuse (IV , inhalational etc) from closed friends
* History of chronic alcohol ingestion
* History of ongoing examination (academic)
* Recently developed depressive illness
* Recent loss of any close family members etc.
As stated earlier, patients of extreme ages almost invariably have organic causes.
History helps in the following ways:
* History of HTN, DM ——–> CVA, DKA, Hypoglycemia
* History of Hypothyroidism (suggested by tàking certain drugs Like Thyroxine)——> Myxedema coma
* History of COPD ———-> Respiratory failure (Carbon dioxide narcosis)
* History of CKD (from drugs or dialysis history)———> Uraemic encephalopathy, Metabolic acidosis etc.
* History of alcoholism ———> Lactic acidosis, delirium tremens etc
* History of BPE (Benign Prostatic Enlargement) and UTI———> Urosepsis (though Acute confusional state, rather than unconsciousness, is likely)
* History of drugs (Specially diuretics) ———>Dyseletrolytaemia (mainly Hyponatraemia)
etc.
Examination findings:
———————————–
* Increased Blood pressure ———> CVA
* Warm periphery, cyanosis, Bounding pulse ———>Respiratory failure (Carbon dioxide narcosis)
* Usually fetid, occasionally sweet Acetone breath (suggested by sweety odour) ———> DKA
* Rapid shallow breathing————> Metabolic (Lactic or others) acidosis
* Fever (may be absent) ——–> Chest infection, Urosepsis etc.
In young male patients:
—————————————
* History of ingestion of poison contained in bottle———–> OPC poisoning
* History of finding empty strips of sedative———-> Benzodiazepine poisoning (Toxicity)
* History of finding alone in a road with lost money bag, watch, cut pockets, torn clothes ———> Transport poisoning
* And history of any organic illness like that of elderly patient (HTN, Type 1 DM, CLD, CRF)———> CVA, Metabolic disorders,
* History of Fever and convulsion———> CNS infections (encephalitis etc)
* History of Alcohol———-> Alcolic, Hepatic encephalopathy etc.
Now, depending on some findings in eye, we can reach these diagnosis:
———————————————————————-
* Bilateral pin point pupils: If unattended = Transport poisoning
* If in the house alone = Pontine Infarction or haemorrhage or Sedative overdose
* Unilateral Ptosis with dilated pupil: 3rd nerve palsy= ICH, ICSOL etc
* Bilateral constricted pupils looking downwards: Thalamic haemorrhage etc
* Mid position, Dilated, Fixed and non reacting to light: Brain stem death.
(Pictures of these changes are attached to the post)
* Fundoscopic examination:
– Massive haemorrhage, flame shaped haemorrhage = Hypertensive encephalopathy
– Roth’s spots = CNS infections (Malaria, sepsis from infective endocarditis etc.)
– Unilateral Papilledema = ICSOL, Massive Unilateral ICH etc.
– Bilateral papilledema = Hypertensive encephalopathy, raised ICP (Intra cranial pressure) due to any cause.
Breathing pattern:
—————————-
* Cheyne-stokes: ICSOL, Narcotic overdose, Brain stem lesion
* Kussmaul: Metabolic acidosis due to any cause, respiratory failure, Hepatic encephalopathy etc.
* Central pontine Hyperventilation: Pontine haemorrhage etc.
Any kind of changes in Breathing pattern should be taken seriously!
Investigation:
———————–
1. Baseline:
– CBC with ESR
– Urine RME
– CXR (Usually portable)
– ECG
– Serum electrolytes
– Renal function tests (Specially , Serum Creatinine and BUN)
– Liver function tests (Specially – – – – Prothrombin time, SGPT, SGOT, Gamma GT etc)
Special:
————-
– Brain emaging (CT, MRI etc)
– EEG
– Blood culture, Urine culture etc
– ABG (Arterial blood gas analysis)
– Toxicological screening
– Viral screening (PCR, ELISA etc)
Depending on the DD and to exclude remote possibilities!
Management:
———————–
1. Symptomatic:
– Put him in semi prone position to avoid aspiration
– Ensure clear Airway, adequate breathing and Circulation
– Evacuate bladder if full (Indwelling catheter may be needed)
– If Poisoning (OPC ) is suspected, remove all clothes maintaining the privacy
– Give any patient (young/old, male/female, Simulated or true coma) due respect and honour
– Never forget to show sympathy and due respect to the attendants
2. Supportive:
– Broadspectrum antibiotic (IV)
– NG tube suctioning or feeding ( Depending upon the clinical conditions and background etiology)
– Oxygen inhalation
– Oropharyngeal suction
3. Specific:
– Depends on final diagnosis:
– Mechanical Ventilation in Respiratory failure
-Specific management of metabolic insults (DKA, Dyseletrolytaemia etc)
-Appropriate antibiotic for sepsis
Rx of raised ICP (Intra cranial pressure) etc.
4. Psychiatric evaluation:
– Specially in cases of Deliberated Self harm (Poisoning and drug abuse)
Counselling:
——————-
1. I have heard all of your complaints and history
2. Im also very much serious about your concerns regarding the patient
3. Depending on preliminary examination I think there may the following possibilities
4. Then describe the possibilities with your rationality
5. Though there may be some other possibilities for which I (we) have to go for certain investigations
6. Then tell the overall prognosis and mortality risk with caution
7. Over enthusiastic attitude should be avoided
8. Allow the attendant to shift to another sophisticated centre if they want to after appropriate counselling. Don’t unnecessarily force them or put them in confusion as an act of scape or relief!
Remember, in other centre there will be none other than your colleagues or friends!
9. Last but not the least, keep faith (along with the respective religious believe of the attendants) on Almighty for final outcome
Some points to remember:
——————————————
* Time is the best medicine in some cases of Unconsciousness. So, WATCHFUL INACTIVITY is a must!
* Shouting to the staff nurses and ward boy should be discouraged. Beacuse, it most often signifies nothing other than the nervousness of the attending Physician
* Counselling should be done not only for once, rather from time to time depending upon new findings, features of deterioration or improvement, new findings in Investigation
* When you are almost certain that the patient is in hypoglycemic coma, (and u dont have CBG strip) dont wait for it. just administer IV glucose. Because, it will not cause any harm to a patient with hyperglycaemia or normoglycaemia. Rather, it will cure him !
* Any kind of rigidity should be avoided during describing the Provisional diagnosis. It can be changed time to time before the final diagnosis is established.
Also, excessive flexibility is not encouraged as it signifies the lack of Confidence and Incompetence of the Physician
* Keep a box of CBG strips only for these kind of patients on admission day
* There is no hurry for measuring the Blood pressure frequently!
* Some doctors (Specially internees and newly placed doctors in wards are found with their BP machine hanging over the shoulder as if BP measurement and control is the ultimate goal. But, is a kind of myth. Actually, u can do a little to control the BP and only little can be achieved by controlling BP in such unconsciousness patients!
* If In Simulated coma, it is a great wastage of time if BP measurement are repeated! You just have to feel the pulse and can hv an idea about the approximate haemodynamic status of the patient.
* Do not criticise the Dx and findings of the previous doctor during counselling
* Unconscious patient should get topmost priority amomg other patients during counselling.
* Try to engage the attendants in supporting management (posture change, eye care, oral care etc.).
My dear doctors, another important aspect I would like to share here.
Scope of Malpractice:
————————————
* Delay in resuscitation (e.g, taking details history from the attendants while keeping the patient over the trolley! !)
* Not briefing the attendants adequately
* Giving all kinds of Ix at a time rather than judicious one
* Teasing the patient with Conversion disorder and not referring them for future psychiatric evaluation
* Negligence in day to day care taking the patient as GONE CASE!
* Unnecessarily shifting the patient to ICU where the case is irreversible one.
Referral:
————–
* Virtually no where! As you are the only (last) hope for them.
* Sometimes, according to the demand of the attendants, you may reffer them to higher centres where relatively more sophisticated and advanced treatment options are available.