প্ল্যাটফর্ম নিউজ, ৯ জুলাই ২০২০, বৃহস্পতিবার
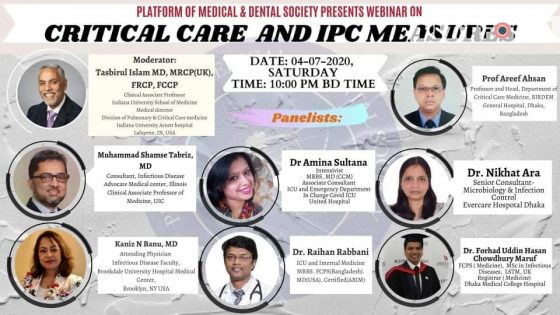
গত ৪ জুলাই শনিবার, প্ল্যাটফর্ম কর্তৃক আয়োজিত কোভিড-১৯ সম্পর্কিত ওয়েবিনার সিরিজের ৩য় পর্ব অনুষ্ঠিত হয়। উক্ত ওয়েবিনারে কোভিড-১৯ এবং এ সময়ের ক্রিটিকাল কেয়ার নিয়ে বিস্তারিতভাবে বিজ্ঞ আলোচকেরা কথা বলেন। এছাড়া দেশব্যাপী জুনিয়র ডাক্তার এবং মেডিক্যাল স্টুডেন্টদের এই সংক্রান্ত নানা প্রশ্নের জবাব দেন বিশেষজ্ঞরা।
এতে মডারেটর হিসেবে ছিলেনঃ
ডা. ফরহাদ উদ্দিন হাসান চৌধুরী মারুফ, এফ.সি.পি.এস. (মেডিসিন),
এম.এস.সি. ইন ইনফেকসাস ডিজিজ,এল এস টি এম, ইউ কে
রেজিস্টার (মেডিসিন),ঢাকা মেডিকেল কলেজ হসপিটাল
প্যানেলিস্ট যারা আলোচনা করেন, তাঁরা হলেন-
১. ডা. মোহাম্মদ শামস তাবরিজ, এম.ডি.
কনসালটেন্ট, ইনফেকসাস ডিজিজ
এডভোকেট মেডিকেল সেন্টার ক্লিনিক্যাল এসোসিয়েট প্রফেসর অফ মেডিসিন, ইউ আই সি
২. ডা. কানিজ এন বানু, এম.ডি.
এটেন্ডিং পিজিসিয়ান,ইনফেকসাস ডিজিজ ফ্যাকাল্টি, ব্রোকডেল ইউনিভারসিটি হসপিটাল মেডিকেল সেন্টার, ব্রোকলেন,এন ওয়াই ইউ এস এ
৩. ডা. আমিনা সুলতানা, ইন্টেনসিভিস্ট
এম.বি.বি.এস. , এম.ডি. ( সি সি এম)
এসোসিয়েট কনসালটেন্ট, আই সি ইউ এন্ড ইমার্জেন্সি ডিপার্টমেন্ট,
ইনচার্জ, কোভিড আই সি ইউ, ইউনাইটেড হসপিটাল।
৪. ডা. রায়হান রাব্বানি
আই সি ইউ এন্ড ইন্টারনাল মেডিসিন,
এম.বি.বি.এস. , এফ.সি.পি.এস. (বাংলাদেশ), এম.ডি. (ইউ এস এ),সার্টিফাইড (এ বি আই এম)
৫. প্রফেসর ডা. আরিফ আহসান
প্রফেসর এন্ড হেড, ডিপার্টমেন্ট অফ ক্রিটিকাল কেয়ার মেডিসিন, বারডেম জেনারেল হসপিটাল, ঢাকা,বাংলাদেশ
৬. ডা. নিখাত আরা
সিনিয়র কনসালটেন্ট, মাইক্রোবায়োলজি এন্ড ইনফেকশন কন্ট্রোল, এভারকেয়ার হসপিটাল ঢাকা
বক্তারা বর্তমান করোনা পরিস্থিতিতে বাংলাদেশ এর ইনফেকশন প্রিভেনশন এবং কন্ট্রোল বিষয়ে আলোচনা করেন। ইংল্যান্ড এর বিভিন্ন হাসপাতালে তাঁরা যেসব অভিজ্ঞতা অর্জন করেছেন, তা শেয়ার করেন এবং গঠনমূলক আলোচনা করেন। আরও যেসব বিষয়ে আলোচনা করেন, তা তুলে ধরা হলোঃ
CRITICAL CARE AND IPC MEASURES
Summarized by
Dr. Tasnia Hamid Kanta, MBBS, DMC
1. Management peculiarities and difficulties in critical care at icu in covid 19 patients?
Areef Hasan
Nearly 20 percent patient needs hospitalization with one quarter needing ICU support.
Mostly they suffer from type 1 respiratory failure, AKI etc.. our main concern is maintaining oxygen saturation stating from Low flow oxygen to high flow. NIV can’t be use due to lack of negative pressure room since it increases the risk of infection.
We also start empirical antibiotic and prophylactic anticoagulation. If suspected mdcbt is done/given.
Convalescent plasma is given. If cytokine storm—tocilizumab.
We are using full PPE. Prism company is helping in disposal.
2. (Dr amina sultana) story behind the struggle of UNITED ICU?
We had some negative pressure rooms which helped in treating the patients initially but later due to increased load, we have to introduce a separate isolation unit. But due to a fire accident it went all wrong. Finally from end of June we were finally able to start a separate icu for covid patient. As a intensivist, we try to prevent invasive ventilation, we currently still lack high flow cannula so here,NIV plays a vital role.
3. (raihan) cause of high mortality in ICU of Bangladesh and what can be done to prevent them?
Actually ICU mortality is generally high. And comparing the health care facilities our ICU hase almost one tenth to those of first world countries.
Tocilizumab is expensive, almost 60k per dose. Not everybody can afford it.
We need to decide in which sector we should expand the health care facilities, IMO, HDU facilities would play a vital role. The cost of a ventilator is equivalent to three HFNC ,later might prove more beneficial in wider range.
4. What are the methods you are taking for prevention of infection?
(nikhat)
– We had an infection control programme since the beginning. It’s a major issue in management of any kind of patients. We have an epidemic plan every year, and this year we adjusted it according to the world covid situation. We divided our patients in critical and non critical areas. Having a common corridor and lift,we had to be extra cautious. We ran regular training programmes for all the staffs. In april our 6 doctors became positive and as a result non critical area was transferred into covid unit. Then a patient was diagnosed as covid pneumonia in critical unit which ultimately led to this covid unit.
We have divided the entire hospital in different zones. Initially patients are receiving treatment in grey zone until their reports came then they were relocated.
Staffs got remarkably affected since May, by the end of the month, almost 75 HCW were becoming affected per day. We had all facilities, and were alarmed.
What we are considering is, it was during Eid time when no lockdown was in action. We could maintain standard environment in hospital but not outside. But with proper diagnosis and isolation, we were finally able to control it. We are treating the staffs free of cost. Even we have introduced institutional quarantine for staffs who are residing at overcrowded area, and thus we are finally able to overcome the fear of doing duty at covid unit. We provided adequate qualitiful mask and ppe. Our main concern is now disposal of ppe. During covid our hand hyigiene compliance were 62 percent which was alarmimg. Main reason was wearing gloves. Even if we were gloves hand hygiene is a must. We trained them and now we hope to see a rise in our july test.
Q: (KANIJ) how did you people prevent the infections in usa?
In NY all hospital are autonomous body. Also it’s a team work. Government and no govt are working together, we assume demand and supply came accordingly. Even our clerks have to attend infection control programmes or else they will get sacked. But to be honest, the patient were overflowed. We got 1000 patient where we were prepared for 100. The reason behind this high infection rate, NY is overly populated, we use public transport most of the time due to limitation of parking. Our homes aren’t well ventilated. And people weren’t aware. So the situation became worse.
We provided care according to sections— mild were managed at home, mostly with telemedicine which decreased the load a lot. A lot patients came already intubated (paramedics at ambulance) , maximum patients came with ARDS and approx. 70-80% patient faced renal failure who needed bed side dialysis. Initially PCR took almost 48 hours, then hospitals started doing rt pcr which reduced the time to 4 hours. We were doing airborne isolation.
Q>>> protocol regarding tocilizumab and anti virals?
IDSA still address supportive mx as the mainstay. We still don’t have any specific antivirals. We administer dexamethasone highest for icu and intubated patients not more than 10 days, if not available, we used methyl prednisolone oral or iv. Initially we were using it for 5 days.
remdesevir is being used in severe not intubated patients. We are still using tocilizumab and plasma therapy. Recent study showed HCQ decreased the mortality in ICU patients but more reports are necessary for the final decision.
it’s not a hospital only management. People should come forward as well. Since it’s a densely populated area, we used hotels, playgrounds, every available facilities for quarantine. We transferred patients to ships who were covid negative. We are now using CDC guidelines for every steps of our life.
Q>>> why in spite of having proper donning doffing,the rate of infection is high. Why so many hcw are infected?(TAZBIR)
actually we can get infected from any kind of breeching . we shouldn’t allow visitors, even if we do so, proper masking is a necessary. Hand hygiene is just as important as oxygen. At Every 15 minutes interval, we need to have a hand sanitizing spot. We need to have some cleaning protocol at least in high touched areas, such as doctors call room,tables,handles,washrooms etc.
we need to make sure no doctor uses his own BP machine or stethoscope , since this personal equipment needs to get very properly disinfected. It can be protocolaized. We can have a disinfection table as well. Measuring BP should be automated now. We should maintain distance at least. But vitals should also be measured so, things should be converted from manual to automated.
we need to have a clean concept about ppe.
like full PPE for a patient with TB is n95 mask and hand hygiene since it doesn’t spread via touch
full PPE for chicken pox is gown, hand hygiene,gloves,n96 mask since it spreads through touch and aerosol. About corona it’s still under evaluation. As far as we know it’s primarily a droplet infection. We need to have a gown, not necessarily a coverall, n95,googles, eye shield. Since its extended droplet infection.
In Bangladesh its really difficult since our ventilation is very very poor so everybody here should use a surgical mask. And due to resource lack, we can try to use surgical mask.
While re using n95 mask , we can use it by protecting it with surgical mask. Also, we can’t bend the metallic part while fixing it. And fixing test in reusing should be done by inhaling a deap breath, to see if it goes backwards.
In USA, we made a temporary doffing area, using polycarbonate material and used fibre glass to separate covid fron non covid unit. In ICU we usually have separate rooms. And all control equipment were kept outside.
and I agree that more than ICU, HDU should be more emphasized. Since MDR infections are so high in our country,death can even be from them rather from covid.
we should and must use separate gowns may it be made of polyester clothings. We are using same PPE for a lot of patients which is an absolute violation of infection control measurement. Our current system is not durable. Maintain distance, proper mask, proper disposal, decrease exposure.
Q. does fogging of goggles indicated a mask isn’t well fitted?
>>> yes, fogging indicates lack in fitting. Trying goggles even can be avoided if N95 is well fitted
TAKE HOME MESSAGE:
AREEF HASAN:
1. INCREASE NUMBER OF HFNC
2. INTRODUCE A CENTRAL MONITORING SYSTEM
3. INTRODUCTION OF TELEMEDICINE
AMINA SULTANA:
1. GIVING A SHORT TERM TRAINING AND INCLUDE PEOPLE FROM DIFFERENT BACKGROUNDS
RAIHAN RABBANI:
1. WE SHOULDN’T VENTILATE UNLESS IXYGEN SAT IS LESS THEN 85%
2. IF ABG FACILITIES IS AVAILABLE , LACTATE LEVEL SHOULD BE CONSIDERED ALSO FOR CHOOSING ICU
3. HFNC ISNT AEROSOL GENERALIZING, WE SHOULD BE MORE CAREFUL IN BIPAP
4.SEPARATE WEBINARS REGARDING EACH AND EVERY OF THIS SHOULD BE INTRODUCED.
NIKHAT ARA:
1.SHARING KNOWLEDGE AND SELF AWARENESS SHOULD BE THE KEY
MUHAMMAD TABRIZ:
YOU PEOPLE ARE DOING A GREAT JOB, IN DEVELOPED COUNTIRES WE GET EVERYTHING READY BUT YOU DON’T. SO MY EARNEST GRATITUDE
2. INTRODUCE A PROPER ANTI INFECTIOUS POLICY ONCE AND FOR ALL, THIS IS THE SCOPE
ওয়েবিনারের সকল আলোচনা থেকে সরাসরি উক্তি তুলে ধরা হয়েছে। প্যানেলিস্টদের বক্তব্যের প্রাসংগিকতা বুঝতে সম্পূর্ণ অনুষ্ঠানটি দেখার অনুরোধ রইলো।
লিংকঃhttps://m.facebook.com/story.php?story_fbid=276849776913995&id=237592689724934

